A lifetime of pain in 24 hours: A French ICU in the pandemic
MARSEILLE, France (AP) — Four more calls to go, each with careful words, painful silences.
It’s 2 p.m. in the intensive care ward of Marseille’s La Timone hospital, and Dr. Julien Carvelli is phoning families hit by the latest coronavirus surge with news about their children, husbands, wives. With intensive care wards at over 95% capacity in France for over 10 days, Carvelli makes at least eight of these difficult calls a day.
In Marseille, this wave is bringing even more people to the ICU than the first one in the spring, many in more severe condition. Carvelli warns one father that his son may need to be put into a coma.
“For the moment, he’s holding on. But it’s true that — I don’t know what you’ve been told already — his respiratory state is worrying,” Carvelli acknowledges. There's a long pause on the other end.
“Listen, do your best,” comes the strained reply.
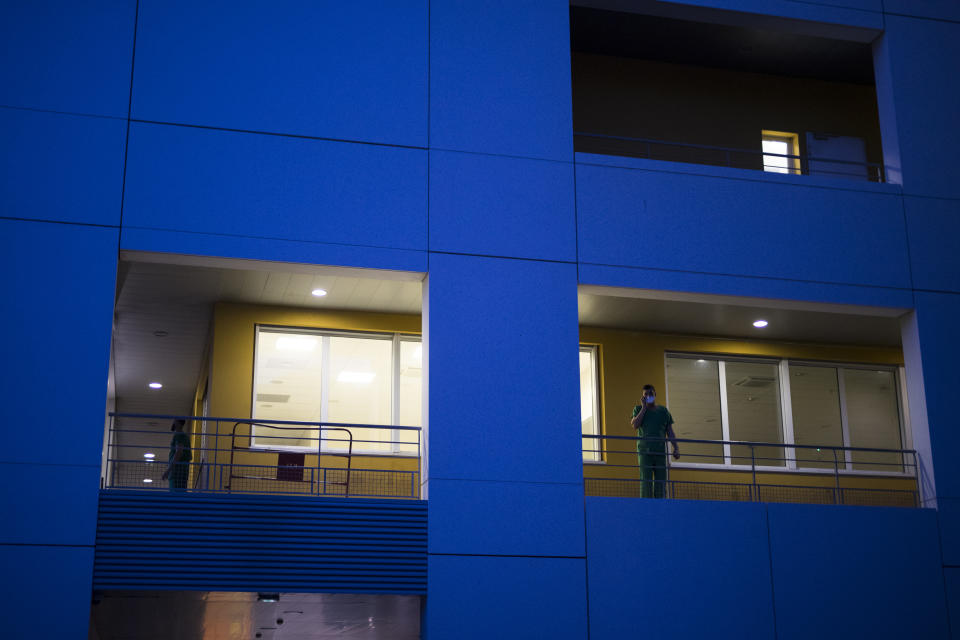
France is two weeks into its second coronavirus lockdown, known as “le confinement.” Associated Press journalists spent 24 hours with the intensive care team at La Timone, southern France’s largest hospital, as they struggled to keep even one bed open for the influx of patients to come.
The doctors and nurses tell themselves and each other that they just have to hold on a little longer. Government tallies show infections may have reached their autumn high point, and hospitalizations dropped last weekend for the first time since September.
But the medical workers are also frustrated that France did not prepare more in the months after the first wave. And while doctors and nurses were seen as heroes back then, this time is different.
“Before, they applauded every night. Now they tell us it’s just doing our job,” says Chloe Gascon, a 23-year-old nurse who has spent half her 18-month career amid the coronavirus. Her voice carries more than a trace of bitterness.
Marseille has been submerged with coronavirus cases since September. The port city, on France’s Mediterranean coast, was spared the worst of the virus last spring only to be hit with a vengeance as summer vacations wound down. Bars and restaurants closed across the city on Sept. 27, more than a month before they shut down nationwide. It wasn’t enough.
A decade of budget cuts left France with half the number of intensive care beds this year, when it needed them most. By the time the first lockdown ended on May 11, more than 26,000 people had died in France. The government pledged to take advantage of the summer lull to add beds and train reinforcements.
That was the time to act, when new infections were at their low point, said Stephen Griffin, a virologist at the University of Leeds.
“It was always bubbling away under the surface,” he said.
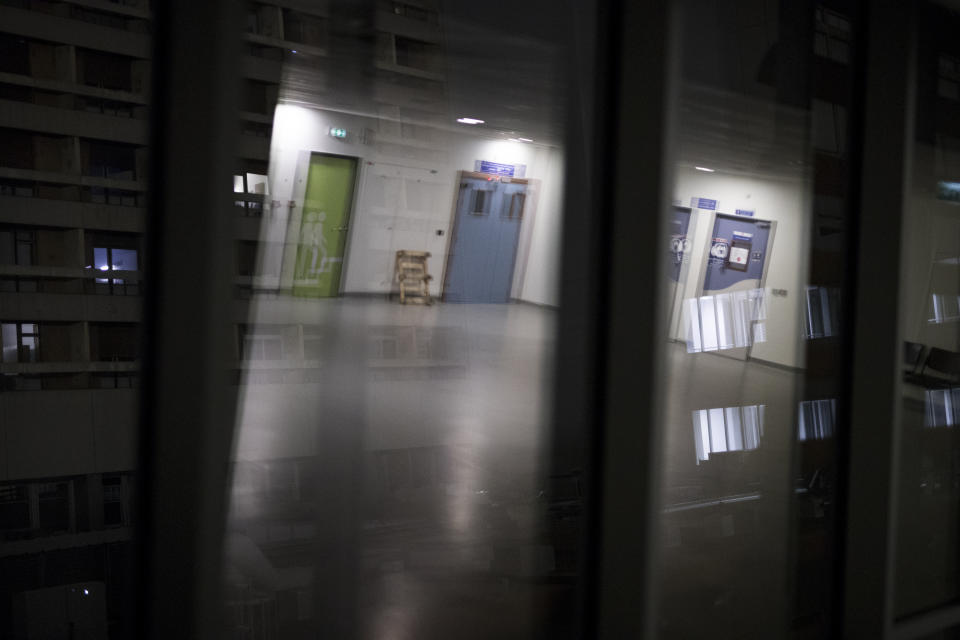
But it was only in early fall that work started on refashioning an acute care wing at La Timone, which opened less than two weeks ago and still has exposed wiring and a fiberboard barricade with duct tape. The promised reinforcements have been slow in coming as well, and any training they get is in the moment, as Pauline Reynier is learning during her first week as an ICU nurse.
Compared to the emergency room, the ICU is a relatively calm place, with moments of urgency when a patient needs more oxygen or an intervention. The quiet is punctuated by the constant soundtrack of machines beeping. There is no good news here; the best news is that a patient is stable enough to be moved elsewhere.
When the 12-hour nursing shift starts at 7 a.m., all 16 beds are filled with COVID-19 patients, and five are conscious. For those in artificial comas, it takes about an hour and at least two people to wash and then carefully rotate each one in their beds, keeping the wires and plastic tubing in place.
This is Reynier’s first task.
She helped in a regular coronavirus ward during the first wave and offered to retrain over the summer for intensive care. Instead, the 26-year-old was sent back to cardiology, which was filling with patients who had postponed heart surgeries. It was just a week into the second lockdown that the call came to report to the ICU on Nov. 11, a national holiday.
It is only Reynier’s second shift as an ICU reinforcement. Her new colleagues barely know her name and have little time to teach. The daughter of a nurse who also works at La Timone, she largely learns by watching.
It takes months to train as an intensive care nurse, years to become experienced in the grueling specialty of holding death at bay.
This virus is even more demanding than the usual urgent challenges. Caregivers risk nearly as much as the patient, and dress accordingly, each time they enter a room. And so going to the bedside means planning multiple tasks at once: washing, toothbrushing, checking vitals, changing IV drips and, finally, turning the patient over to help improve breathing.
Reynier pulls on a long-sleeved apron over the scrubs with a quick twist of the wrist to knot the neck. Then a pair of gloves. Punches a thumbhole through the bottom of the sleeve to secure the gloves, then pulls on a second pair of gloves. Head covering, goggles and, finally, a second apron in plastic. X-ray technicians wear a third set of gloves to handle the plates. Doctors performing an intubation or other major procedure wear a plastic face shield over the goggles.
For every person inside the room, someone stands on the outside to hand over anything needed and help strip off and discard the protective gear at the end. Every gesture takes on outsized importance.
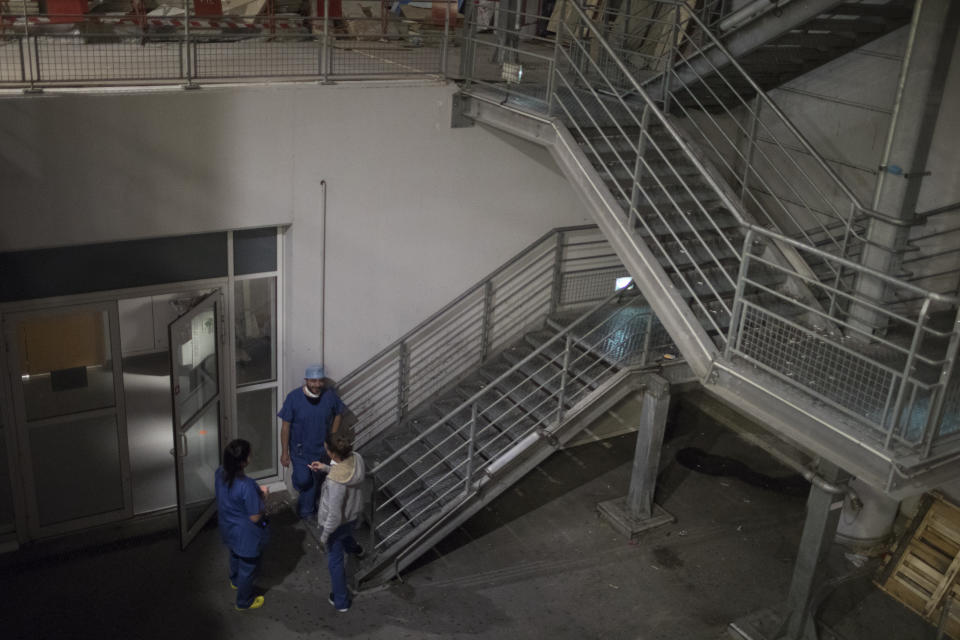
Mid-morning, the man in Room 6 improves enough to go to acute care. At the same time, doctors realize that Room 11 in the makeshift ward isn’t equipped for the dialysis machine that the unconscious patient inside now urgently needs. He has to be moved across the hall to the main ICU.
Doctors and nurses snatch aprons, gloves and goggles off the cart outside to swaddle themselves.
It’s about 25 meters (yards) away — a quick left, through two sets of double doors, past the break room and the workstation. Moving the 60-year-old man ultimately requires 14 medical workers and 45 minutes of preparation — including hooking him up to a portable oxygen generator that later must be disinfected.
They start moving the bed at 10:40 a.m. It takes 15 minutes to maneuver him into position in Room 6. Sweat darkens the back of Reynier’s pale blue scrubs.
A cleaning crew storms Room 12, filling it with the smell of bleach: One bed is now free.
It is 1:30 p.m. and many of the nurses are in the windowless breakroom. The doctors have converged on Room 9, just outside. The 54-year-old man was conscious in the morning, but his oxygen levels are dropping and it's time to sedate and intubate him.
Again, doctors and nurses converge, three people inside and three outside Room 9 to fetch tubing, scissors, bandages. The doctors replace an IV in the man’s right arm and gently cover his torso with the sheet when they’re done, an hour later. Now, all but four of the 16 coronavirus patients are in artificial comas.
“We just have to help them to hold on until their bodies can heal,” Carvelli says. “But intensive care is a terrible thing in itself. Not everyone can survive it.”
This is not what he tells families during the half-hour or so he spends calling them each day. Each call is over in minutes.
“We have to be reassuring and at the same time tell the truth. It’s a balance that is sometimes hard to find,” Carvelli says quietly.
There's a silver lining to a very dark cloud: This time around, doctors have learned enough about the disease that they know when a patient is about to die and can summon families to the ICU. That's what happened at La Timone last week.
During the daily calls, families ask about the most recent coronavirus test — patients are tested three times each week — about oxygen levels, sedatives.
“You know, even if he tests negative, it doesn’t mean he will heal more quickly,” Carvelli gently tells the daughter of a man in the ICU for four days.
"No, it’s just that if he doesn’t have COVID, it’s one less thing,” she replies.
The man is still positive, but Carvelli tells her he is conscious.
“Can you tell him we are here and we support him?” she asks.
“Of course.”
Her voice breaks as she says goodbye.
The disease is taking its toll on the staff as well. No doctors and only a few nurses have been infected at La Timone, but they are exhausted.
At 4:30 p.m., two hospital managers come down, in part to gauge morale. Marie-Laure Satta, at 37 one of the senior nurses, confronts them testily, with Reynier looking a little lost at her side. The younger woman has just learned that she’ll be returning to the ICU for at least the next few weeks, and she is both relieved and worried.
The reinforcements need checklists, written instructions, something tangible to guide them so they’re a help to the regular staff, not a burden, Satta says, her entire body tense with emotion.
“I’m talking about well-meaning people who are here to aid, who just need a little reminder,” she snaps. “We need some rest.”
The managers understand, but it’s not clear how much control they have over the situation. The conversation ends cordially even so, and they make their way out of the ICU.
“Good luck to you too, because you’re not in any better position than we are,” Satta calls after them.
Like all the caregivers at La Timone, Satta is completely dedicated during the greatest medical crisis of her generation. But she yearns for something less stressful once this is over, maybe helping to arrange organ transplants.
Her husband works the night shift at the ICU and they have two children in preschool. Neighbors help out with the childcare gaps, which tend to be in the morning and late afternoon. She believes the promises of the government are empty.
“They serve other interests than the comings and goings of a hospital. I’ve never seen that, either for the patients or the caregivers," she says when the mood has calmed. “With all of France’s capacity, all of France’s money ... they talk to us about savings — where does all that money go?”
Marseille was once one of the world’s richest cities, its natural harbor an international hub dating back to 600 B.C. and its founding by Greeks of Phocaea. The city is in a waterfront depression ringed by limestone hills, with La Timone almost straddling its central axis.
Many historians believe the first wave of the Black Plague in Europe originated in Marseille's port. The continent’s last major Plague outbreak, in 1720, killed half the city’s population. Local schoolchildren visit the Frioul archipelago, 4 kilometers off the coast, and the H?pital Caroline, which cared for sailors with the Plague.
“What we’re going through now will be studied in history, because it’s exceptional,” Reynier tells her new colleagues.
By now, the day shift is nearly over. The bed in Room 12 is still free, and the physician overseeing the night shift hopes to keep it in reserve, to keep just a little slack in the overloaded health system.
“I want to keep a bullet in my chamber,” Dr. Fouad Bouzana says, between phone calls from other hospitals asking about open beds. La Timone’s emergency room calls, asking for space for a man who is COVID-19 positive. Bouzana asks them to run more tests and call back.
The ICU doesn’t accept everyone. Doctors learned in the first wave that coronavirus patients need a certain base level of strength and health to make it through the recovery.
That night, Bouzana turns two coronavirus patients away, deeming them too elderly and frail to submit to intensive care. They’ll stay in the acute care ward next door in hopes their condition improves, and he’ll review the decision with the dayside doctors later. But he harbors little doubt.
“We discuss it together. If one of us wants to take a patient and the others don’t, we always take the patient,” he says. “We usually agree.”
At 2 a.m., the man from the emergency room is admitted to the last remaining bed.
La Timone is full again.
___
Follow AP’s coverage at https://apnews.com/hub/coronavirus-pandemic and https://apnews.com/UnderstandingtheOutbreak