What Does Cellulitis Look Like?
A Common Infection of the Skin
Medically reviewed by Isaac O. Opole, MD, PhD
Cellulitis is a common infection of the skin, almost always caused by bacteria. The infection can come on suddenly and usually spreads from the skin surface (epidermis) and then goes deeper into the dermis and the subcutaneous fat layers.
Cellulitis can cause redness, skin swelling, pain, heat at the site, and possibly fever. It is not contagious and typically affects only one site in the body (for example, just one leg) at a time.
This article explains the symptoms and causes of cellulitis. It discusses how your healthcare provider can treat cellulitis (typically with antibiotics) as well as complications that may require further care.
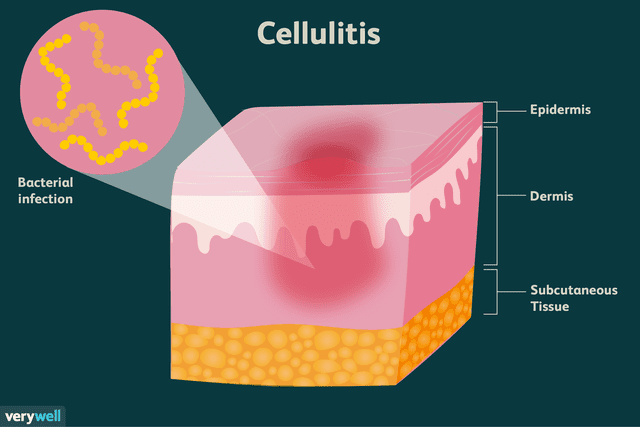
Illustration by Alexandra Gordon for Verywell Health
What Are the Symptoms of Cellulitis?
Cellulitis symptoms include redness, swelling, and pain in the skin. Cellulitis often gives skin a pitted appearance, similar to an orange peel. It can also cause the skin to blister and peel. While cellulitis can occur anywhere on the body, it is most common on:
The feet
Lower legs (about 70% to 80% of cases)
Arms (cellulitis is often associated with breast cancer treatment)
A serious bacterial infection of the skin, if left untreated, cellulitis can spread and cause serious health problems. If you have symptoms of cellulitis, see your healthcare provider.
Pictures of What Cellulitis Looks Like
The following pictures of cellulitis on legs and feet offer a sense of how affected skin may look in both early stages and further on.

DR P. MARAZZI / SCIENCE PHOTO LIBRARY / Getty Images

Wendy Townrow / Getty Images

Reproduced with permission from ? DermNet New Zealand www.dermnetnz.org 2023.

Wendy Townrow / Getty Images

LagunaticPhoto / Getty Images
What Are the Causes of Cellulitis?
Cellulitis occurs when bacteria enter a break in the skin. This could be a nick, cut, or tear caused by an injury, surgery, bug bite, burn, or itching of a rash. It could also be a breakdown of the skin's integrity due to a skin condition like eczema or athlete’s foot.
It can affect those who have swelling in their legs due to venous stasis, or lymphedema after surgery for breast cancer. People with varicose veins (as well vein stripping or ligation procedures to treat them), or vein grafts taken for other surgeries, cannot clear bacterial infection as quickly and tend to have more cases of cellulitis.
Cellulitis is more common in older adults but can happen in any age group and either gender. A 2017 study also found that when cellulitis occurs, it is more likely to be severe in older people.
Who's at Risk for Cellulitis?
Certain conditions can increase the risk of cellulitis. Diabetes, for example, makes both infection and cellulitis complications more likely. Other factors and conditions that increase risk include:
Age
Obesity
Varicose veins (or certain surgical treatments for them)
Chronic leg edema (swelling), as with heart failure
Alcohol misuse and liver cirrhosis
Immune system compromise
Breast cancer treatment (leading to lymphedema)
Foot checks performed by a healthcare provider are important in those with diabetic neuropathy to make sure they don’t have any skin breakdown, ulcers, or wounds if they can’t see for themselves.
Types of Cellulitis
Cellulitis infections are often caused by the bacteria Staphylococcus aureus (including methicillin-resistant Staphylococcus aureus known as MRSA) and Group A Streptococcus. Many cases of Staph aureus are now resistant to the antibiotics that once worked.
Related: Difference Between MRSA and Staph Infection
Rare Types
There are a few rare causes of less common types of cellulitis. Some of these can be dangerous in those at risk—such as those who are immunosuppressed, have diabetes, lack a spleen, or have liver problems.
Cat bites, which can be deep and more dangerous than commonly realized, can introduce Pasteurella multocida, leading to serious infections of the skin and deeper structures. Dog bites can in rare cases lead to a serious cause of the infection Capnocytophaga, which is very dangerous in those who do not have spleens.
Exposure to warm salt water, such as from a walk on the beach, especially in those with liver or alcohol problems, can lead to Vibrio vulnificus. This is a serious infection which can be fatal if not quickly treated.
Freshwater exposure can be associated with Aeromonas hydrophila infections. Children sometimes have infections with Haemophilus influenza.
Surgery can lead to cellulitis, even rare types like mycobacterial infections. Those who are immunocompromised can be prone to a wide range of infections, like Pseudomonas, Proteus, Fusarium, and Serratia.
Those at risk may require different antibiotics upfront, even though most cellulitis cases are caused by either Staph or Strep infections.
How Is Cellulitis Diagnosed?
Cellulitis is usually diagnosed based on its appearance, but certain tests may be used to confirm a diagnosis, inform decisions about treatment, or evaluate how treatments have worked. This includes:
Blood testing: Sometimes healthcare providers will check a person’s blood count to see if the white blood cells are elevated (meaning that the immune system is fighting an infection). That said, an elevated white blood cell count may not occur in the early stages of an infection. In people who are very ill, blood cultures may be performed to see if the bacteria has spread into the bloodstream. Unfortunately, cultures are only positive in 5% to 13% of cases, making a definitive diagnosis difficult.
Aspiration: Less commonly, a healthcare provider may opt to perform an aspiration, which involves the injection of sterile fluid into the infected tissue, after which fluids are drawn out in the hopes of capturing some of the bacteria. This is usually done only in extreme cases since aspirations may return inconclusive results.
A skin biopsy culture: During this procedure, a small sample of the affected skin is removed and placed in a petri dish to see if bacteria grow. This may be performed if the diagnosis is uncertain and/or to rule out diagnoses that can mimic cellulitis, like a drug reaction or vasculitis.
Imaging tests: An ultrasound or magnetic resonance imaging (MRI), may be used to distinguish cellulitis from another diagnosis, like a deep venous thrombosis (DVT) or osteomyelitis (a bone infection).
How Is Cellulitis Treated?
Treatment usually consists of oral antibiotics. Most people get better quickly and do not require hospitalization.
Because it is uncommon for people with cellulitis to discover the exact type of bacteria causing the infection (there is rarely any testing performed to show which type of bacteria is responsible), healthcare providers often have to make educated guesses about what the likeliest bacteria are and base treatment on the hypothesis. This is called empiric therapy.
Using empiric therapy, antibiotics are selected by the healthcare provider to cover the most likely types of bacteria, depending on what specific risks the patient has. Because MRSA can cause cellulitis but is often resistant to common antibiotics, empiric antibiotics treating MRSA are sometimes given to people with cellulitis to increase the chance that antibiotics will work.
A healthcare provider may mark the borders of the infection to monitor its growth. They also may elevate a body part to help with drainage while expecting the infection to recede in a day or two.
However, if someone becomes more ill or febrile (feverish), or the infection is not diminishing, they may need to be hospitalized and may need IV antibiotics.
What Are the Complications of Cellulitis?
Several complications may arise as a result of cellulitis.
Abscesses
Abscesses can form from severe infections. An abscess is a pocket of infection that can be difficult to clear. It may need drainage and not just antibiotics.
Orbital Cellulitis
Orbital cellulitis, which is more common in children, can occur when bacteria spread to the areas around the eye (behind the orbital septum). Any pain with moving the eye, inability to open the eye, infection around the eye, or swelling of the eyelid should be taken seriously.
This type of cellulitis usually involves the spread of bacteria from cellulitis in front and around the eye or from the sinuses (or bloodstream) to the eye socket. It is not the same as periorbital cellulitis, which refers to an infection only in front of the eye and not deeper into the eye socket.
Orbital cellulitis is a serious infection which can lead to loss of sight and even the spread of bacteria to the meninges or brain.
Necrotizing Fasciitis
Necrotizing fasciitis is a rare infection of the deeper layers of skin, reaching down to the fascia below. It causes extreme pain and can spread very quickly. It can quickly lead to the death of the tissues in these layers (subcutaneous and fascia), and in turn lead to the death of the patient, especially if treatment (surgery and antibiotics) is not rapidly available.
Sepsis
Sepsis can occur when the bacteria from the skin reach deeper and spread through the blood, seeding other parts of the body. This can be very serious, requiring hospitalization and IV antibiotics.
How Is Cellulitis Prevented?
The best prevention of cellulitis is to take care of any break in the skin, which includes:
Washing the wound daily with soap and water
Applying a topical antibiotic to the wound
Keeping the wound covered with a bandage
Changing the bandage daily (or more often if it gets dirty or wet)
Learn More: How to Properly Dress a Wound
It's also important to address with your healthcare provider any underlying health condition that increases your risk for developing cellulitis, such as poorly controlled diabetes, obesity, or extremely dry skin.
When to Seek Urgent Care
Cellulitis can be an urgent medical concern. Seek immediate medical attention for cellulitis if the red area of the skin expands quickly or you experience fever or chills. Other symptoms of severe cellulitis, or related complications such as sepsis, can include:
Dehydration
Low blood pressure
Confusion
Shortness of breath
You should contact your healthcare provider if cellulitis treatments haven't worked. If skin tissue appears like it's dying (necrosis) or organs aren't functioning well (like the kidneys), seek care.
Keep in mind that older people may be more at risk for infection. Underlying health conditions also can contribute to the need for urgent care; diabetes, for example, presents five times the risk of sepsis or other complications.
Summary
Cellulitis is a skin infection that comes on quickly and can turn serious. While some bacteria live on the skin at all times and are generally harmless, if they enter the skin, they can cause infection.
If you notice any swelling, redness, pain, or heat at a site where you’ve had a cut, bite, or burn on your body, seek medical care immediately.
Frequently Asked Questions
Can cellulitis go away on its own?
No. Cellulitis is a bacterial infection that requires treatment with antibiotics.
What gets mistaken for cellulitis?
Conditions that can be mistaken for cellulitis include:
Irritant dermatitis
Lipodermatosclerosis
Lymphedema
Venous eczema
Read the original article on Verywell Health.
