3 COVID-19 vaccines to start human trials this summer: Here’s what that means
UPDATE 6/10/20: The National Institutes of Health will be funding trials of three experimental vaccines, slated to begin phase 3 trials this summer, according to the Wall Street Journal. The first will be piloted by Moderna, followed by Oxford/AstraZeneca and Johnson & Johnson. In an interview with CNN, Director of the National Institute of Allergy and Infectious Diseases Dr. Anthony Fauci expressed optimism. "The coronavirus vaccine effort is progressing very well and we expect more than one candidate vaccine to be in advanced clinical testing by early summer," Fauci said.
UPDATE 5/12/20: While testifying in front of a Senate committee on Tuesday, NIAID Director Dr. Anthony Fauci said that he is hopeful a vaccine will be entering advanced trials by late fall or early winter. At least eight potential coronavirus vaccines, Fauci confirmed, are now in development.
-----------------------------------------------------------------------------------
President Trump announced on “Fox News Sunday” that he believes there will be a way to prevent coronavirus infections by December. “We think we'll have a vaccine by the end of this year and we're pushing very hard,” Trump said. “We’re building supply lines, we even have the final vaccine.”
The Ebola vaccine, which took four years to create and approve, remains the fastest amount of time that a vaccine was developed. Trump is aiming to fix that with “Operation Warp Speed,” a joint effort between the Department of Health and Human Services and the Food and Drug Administration. But although the president seems confident that a vaccine is imminent, members of the White House Coronavirus Task Force had suggested that the timeline for a vaccine will likely be between 12 and 18 months.
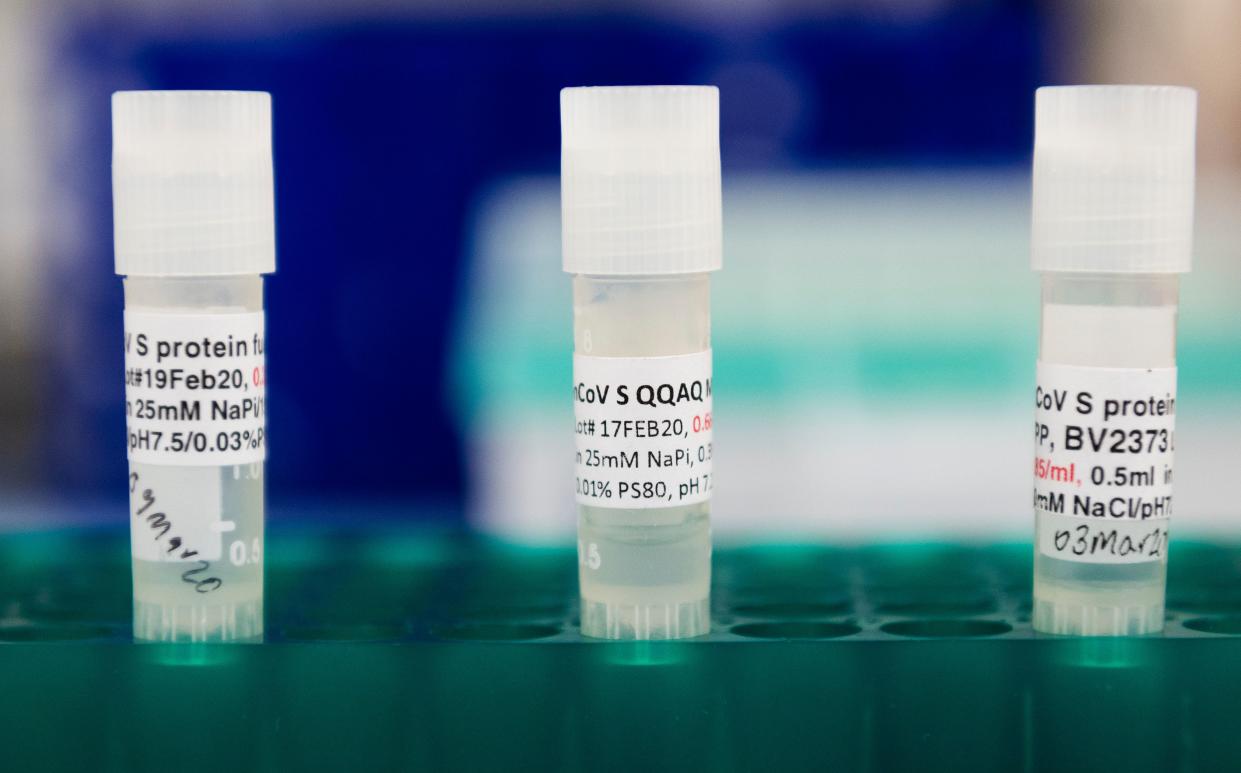
The timeline isn’t the only confusing aspect of the race for a cure. With more than 90 vaccines being explored across the globe, six of which have begun testing on humans, it’s difficult to keep up with the process. Yahoo Life spoke with Dr. Gregory Poland, head of the Mayo Clinic's Vaccine Research Group, to help unpack the process, and clarify why earning vaccine approval is deliberately difficult.
Vaccine development requires funding, then rigorous clinical trials
Poland says the process begins with “pre-clinical work,” which requires securing funding — either from the National Institutes of Health or another investor — followed by “small-animal testing” studies. After these are completed, researchers can submit for FDA approval to begin human testing. As of April 30, at least six companies have won this approval, allowing them to enter the clinical phase of vaccine development. This is a three-step process of testing it on humans. Phase 3, the final and largest test, hinges on gathering proof that the vaccine is safe. Poland says this is inarguably the biggest obstacle.
“This movement from phase 2 to phase 3 is called affectionately the ‘valley of death’ because the vast majority will not make it through phase 3,” says Poland. “Medical literature is littered with things like this. One company bet their entire [worth] on a herpes simplex vaccine and in phase 3 found out they were wrong and they went out of business.” As of now, no companies have passed phase 2 trials for the COVID-19 vaccine.
After phase 3, the vaccine must undergo a regulatory review
Companies that complete phase 3 trials submit their work to a committee run by the FDA’s Center for Biologics Evaluation and Research External. This team of vaccine experts — which often includes Poland — reviews the research to determine if the vaccine actually protects people from the pathogen and is safe. Poland says that if the FDA decides to approve this vaccine, it usually requests a phase 4 clinical trial to be conducted while the vaccine is being manufactured. This involves giving the vaccine to “hundreds of thousands to millions” of individuals to ensure nothing “unusual is happening.” Even once a vaccine is released, the FDA monitors side effects through a database known as the Vaccine Adverse Event Reporting System, as well as investigates the manufacturing facility.
The process is intentionally extensive to protect the public
“There is a reason this is slow, reflective, deliberative, evidence-based peer-reviewed,” says Poland. “Think of what we’re fundamentally doing — we're going to give a biologic to a completely healthy person to hopefully prevent a disease they may or may not get exposed to. So the safety bar necessarily has to be very high.” If Operation Warp Speed pushes a vaccine through clinical trials by the fall — which Poland says is unlikely — he imagines the vaccine wouldn’t be out until 2021. But even then, he says it would be an unprecedented and potentially risky move. “It will be a vaccine that has not been tested according to the same pathway that previous vaccines have been tested,” says Poland.
There is a faster, high-risk option known as “human challenge studies”
Poland says that in rare cases, vaccinologists can take an alternate route to approval through what’s known as human challenge studies. “We’d take young volunteers, give them the vaccine, sequester them in a facility, and then deliberately expose them to virus today,” Poland explains. “As you might imagine, if we could do that 20 or 40 times and everybody did just fine with no side effect and no disease, we know something that otherwise takes seven years to figure out. The question is, is it safe and is it ethical to do that?” He says the malaria vaccine is a recent example of this being process used.
Although there is no evidence that human challenge studies are underway for a coronavirus vaccine, three experts argued in a March paper — published in the Journal of Infectious Diseases — that it’s the best path forward. “Controlled human challenge trials of SARS-CoV-2 vaccine candidates could accelerate the testing and potential rollout of efficacious vaccines,” the authors write. “By replacing conventional phase 3 testing of vaccine candidates, such trials may subtract many months from the licensure process, making efficacious vaccines available more quickly.” The authors note that the move is potentially dangerous, with risks including “severe disease and possibly even death,” but say that such a study could “reduce the global burden of coronavirus-related mortality and morbidity.”
It’s too soon to have confidence in any of the vaccine candidates
The press, the public and politicians have quickly latched onto any rumbling of success from the more than 90 companies currently exploring vaccines. Among those that have emerged as front-runners are Moderna, a U.S. drugmaker working on a vaccine that is currently conducting phase 1 trials, Inovio, another U.S. company in phase 1 trials and Beijing-based drugmaker CanSino Biological, which has reportedly entered phase 2. Johnson & Johnson and Pfizer are also racing ahead with their own vaccine candidates, reportedly planning to enter clinical trials this fall.
Although it may be tempting to jump to conclusions about the clinical testing of these vaccines, Poland likens that to “swinging from one moonshot to another.” As someone steeped in this work, he suggests Americans consider the race for a vaccine through the lens of the popular fable “The Tortoise and the Hare” instead. “The moral of the story,” he says, “is that the race does not always belong to the hare.”
Correction: This story was originally published on May 4, 2020 at 4:47 p.m. ET and incorrectly stated that HHS spokesman Michael Caputo had capped the vaccine timeline at 18 months. It has been updated to note that members of the White House Coronavirus Task Force have spoken of a 12-to-18-month timeline for the vaccine (including HHS Secretary Alex Azar and NIAID Director Dr. Anthony Fauci).
For the latest coronavirus news and updates, follow along at https://news.yahoo.com/coronavirus. According to experts, people over 60 and those who are immunocompromised continue to be the most at risk. If you have questions, please reference the CDC’s and WHO’s resource guides.
How to maintain your physical and mental health during the pandemic
Taking care of a loved one with COVID-19? Here’s how to stay healthy
Q&A with Dr. Kavita Patel: How to keep your family safe and maintain your mental health
Read more from Yahoo Life
How a free, extremely low-risk ER procedure is saving lives from coronavirus
As Georgia reopens nail and hair salons, lawyers say companies may be putting themselves at risk
Retirement home throws emotional social distancing parade for residents: 'I'm still on cloud 9'
Want daily lifestyle and wellness news delivered to your inbox? Sign up here for Yahoo Life’s newsletter.

