Soaring congenital syphilis rates in US risk lives of thousands of babies

Health advocates are calling on the Biden administration to declare a public health emergency over a steep rise in congenital syphilis cases. The easily treated infection has quintupled in 10 years and can have harrowing impacts on children.
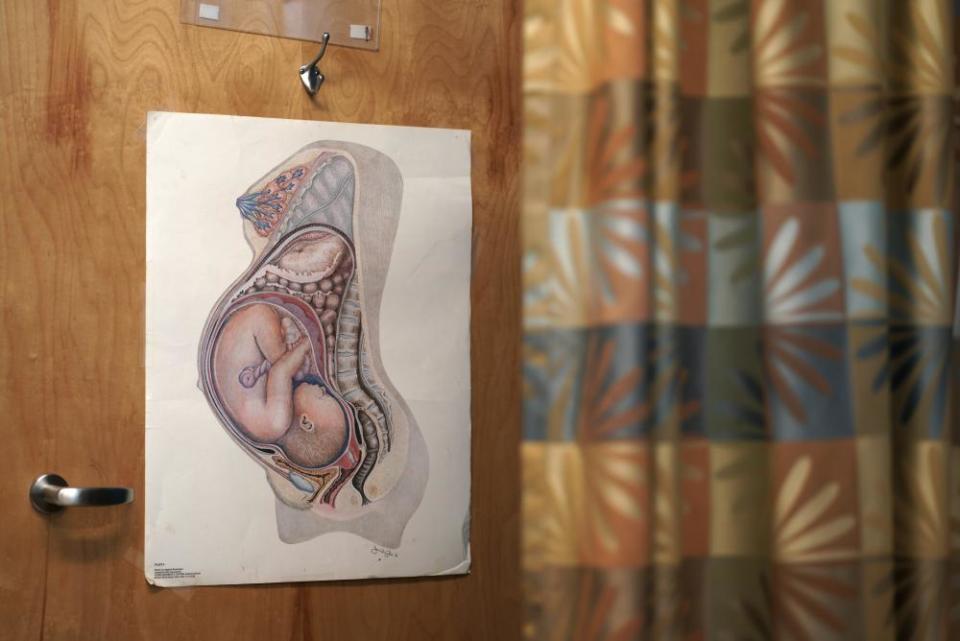
Congenital syphilis happens when a baby contracts syphilis from its mother. Up to 40% of babies born to untreated mothers will be stillborn or die. Others can be left with severe birth defects such as bone damage, anemia, blindness or deafness, and “neurological devastation”.
Related: US approves first RSV vaccine for use during pregnancy to protect babies
“There is not a single baby that should be born in the US with syphilis,” David Harvey, the executive director of the National Coalition of STD Directors, told the Guardian. “We will be judged very severely as a country and a society for allowing this to happen to babies, when it is so easy to diagnose, treat and prevent this disease.”
Rates of the disease have reached a nearly 30-year high just as supplies of the preferred medication, called Bicillin L-A, are in short supply. Syphilis can be cured with between one and three shots of the medication.
Pfizer is the only manufacturer of the medication, a form of the first antibiotic ever synthesized, penicillin. The company said it does not expect shortages to be resolved before 2024, and blamed low supply partly on the increase in syphilis cases.
That has led public health leaders to make the “uncomfortable” choice to direct the medication almost exclusively to pregnant patients. Bicillin L-A is the only drug known to safely treat syphilis in pregnancy, and is so critical to treatment of the pregnant person and fetus that even people with penicillin allergies will receive the drug after being sensitized to it by an allergist.
Problematically, it also means others must rely on doxycycline, an antibiotic that must be taken twice daily for at least 14 days, a schedule some patients will struggle to adhere to. Men who have sex with men are more likely to be diagnosed with syphilis. As a result, the Bicillin shortage is most likely to hit the LGBTQ+ community hardest.
“This is a direct reflection of an ailing public health system,” said Harvey. “We have the highest sexually transmitted infection rates in the western industrialized world, and it is a crisis in the US.”
Syphilis is among a group of sexually transmitted infections (STIs) tracked by the government – including chlamydia, gonorrhea and HIV – all of which are on the rise. From 2020-2021, amid the disruptions caused by the pandemic, the US saw a 30.5% increase in congenital syphilis cases.
The dramatic increase is not due to the pandemic alone. Syphilis was nearly eradicated in the early 1990s, as the HIV epidemic raised public awareness of the perils of STIs, but the disease has made a return amid stagnant and siloed public health funding.
Harvey called on the Biden administration to declare a public health emergency and use the Defense Production Act to manufacture more Bicillin in the US. Further, a coalition of 38 public health organizations this month called on the White House drug shortage taskforce to investigate the shortage.
A spokesperson for the Department of Health and Human Services (HHS) said that the administration had already “established a federal taskforce dedicated to spearheading a national syphilis and congenital syphilis public health response” earlier this year, and that the taskforce had a mission to address the intertwined issues, “reduce their rates, and promote health equity”. The taskforce is also prioritizing “technical assistance and other resources” for a dozen of the most hard-hit places in the US.
A White House spokesperson said the administration remained focused on “critical supply chains” and has already issued five executive orders with the goal of strengthening them.
“This work to strengthen pharmaceutical supply chains is a continuation of the work that began on day one of President Biden’s administration to ensure Americans can access the medicine they need when they need it,” a White House spokesperson told the Guardian.
However, public health officials in the regions hardest hit believe more needs to be done to address a “spike” in cases that may only be the beginning. Mississippi’s high rate of congenital syphilis has received particular attention, thanks to the research of Drs Manuela Staneva, Charlotte V Hobbs and Thomas Dobbs.
“It is a national issue, and I think our work on this issue in Mississippi is just the tip of the iceberg,” said Dobbs, the dean of the John D Bower School of Population Health at the University of Mississippi medical center. Dobbs said the situation was “absolutely” a public health emergency, though he stopped short of calling for an official declaration.
“There need to be national efforts, whatever construct,” he said.
In 2021, US rates of congenital syphilis reached 77 cases for every 100,000 live births, or 2,855 cases. By comparison, the United Kingdom reported 11 cases in five years from 2014 to 2019, the most recent year for which data is available. Because the UK had no cases in 2019, its effective rate is 0 per 100,000, according to the World Health Organization.
At the same time, the US national rate obscures wildly uneven regional distribution of congenital syphilis in the US. Babies in the south-west and deep south – representing border states and states where healthcare is most difficult to access – are born with rates of congenital syphilis far higher than those in the rest of the country.
Mississippi saw a 74.5% “spike” in cases between 2020 and 2021. The state’s rate of 184 cases per 100,000 live births look more like they do in Haiti (181 cases per 100,000) than they do in the US nationally. However, the highest rates in the nation are in Arizona, where health authorities reported 232 cases per 100,000 live births.
The national rate also obscures places where there are few cases of syphilis – Maine, New Hampshire, Vermont and Wyoming have all but eliminated congenital syphilis. Each has had zero or just one case in five years.
Studies like those by researchers in Mississippi blame intersecting factors for the rise in syphilis in the deep south and south-west, beginning with funding. The majority of funds to prevent and treat STIs come from the federal government. But since 2003 funding has remained flat, and thus lost 40% of its purchasing power to inflation.
In just one example, health departments suffered a shock when the administration agreed to claw back $400m in Centers for Disease Control and Prevention funds that could have been used for disease intervention specialists – workers who find patients with STIs and break the chain of infection. The administration made the agreement this summer under pressure to reach a deal on the debt ceiling.
Federal funding silos have also made it difficult to direct money where it’s needed in real time. In one case, silos and lack of state funds led an HIV clinic in southern Mississippi to close – with the nearest clinic being 75 miles away, Dobbs reported in the journal Health Affairs.
“It’s a perfect storm for increase in syphilis in years to come,” said Hobbs. “In adults, in mothers and, of course, unfortunately in children.”
